When measuring the success of migraine treatment, it is easy to focus on clinical features like attack frequency. It is crucial not to forget the person behind the migraine, said Professor Dawn Buse of the Albert Einstein College of Medicine, New York, at a symposium at the AHS 2022 hybrid meeting in Denver.
The detrimental impact of migraine on meaningful parts of everyday life is well-known, not only for patients themselves, but also their families.1 Yet Professor Buse shared that in her experience, patients face a long and difficult path from their first migraine attacks to specialist care.
Chronification leads to worse disability
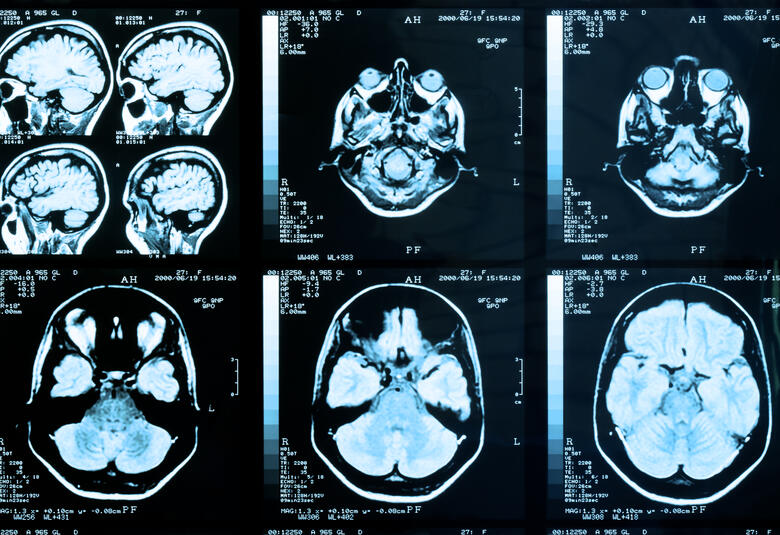
This lack of refined treatment can lead to migraine chronification.2 A key risk factor for chronification is medication overuse and the vicious cycle it can set in motion.3 Chronification has pathophysiological consequences including changes in brain structure and function,4,5 leading to worse clinical outcomes, such as increased symptom severity.6
Three times as many patients with chronic migraine had moderate or severe disability compared with episodic migraine7
These consequences result in a higher disease burden. A real-world study of 634 Japanese patients with migraine collected patient-reported headache-related disability using the Migraine Disability Assessment (MIDAS) questionnaire. There were significantly more patients with moderate or severe MIDAS scores with chronic migraine compared with episodic migraine (60.0% versus 21.0%, p < 0.001).7
Consider disability when assessing treatment needs
The recent American Headache Society (AHS) 2021 Consensus Statement places a high importance on disability when considering preventive treatment. Their criteria for preventive treatment include significant disruption of daily life despite acute treatment. In addition, their threshold of number of headache days per month at which to consider preventive treatment decreases with increasing degree of disability, as measured by a validated tool such as MIDAS.8
AHS guidelines emphasize disability when considering preventive treatment8
Including the patient is vital
To maximize the chances of successful treatment, it is critical to ensure treatment goals are personalized for each patient.8 In particular, care should be taken to include patient needs, which may be different from the clinician’s goals.
Clinician’s goals can include reducing attack frequency and severity and use of acute treatments, and improving quality of life.8 Patients may express additional needs such as a rapid onset of action or lack of side effects.9
The treat-to-target approach includes patients in decisions and disease assessments10
The concept of “treat-to-target”, used in rheumatoid arthritis, can equally be applied to treatment of headache disorders. Treat-to-target prioritizes shared decision-making between the clinician and the patient. In addition, the disease status must be measured often and the treatment adjusted to make sure the goals are reached.10 Patient-reported outcomes can be a very important part of measuring treatment effectiveness.11
Anti-CGRP treatments offer hope for hard-to-treat patients12
Hope for improved patient outcomes
Recently emerging treatments give reason to be optimistic. Treatments targeting calcitonin gene-related peptide (CGRP) offer a new treatment option, in particular for patients that are hard to treat.12 In the future, more nuanced approaches may be possible with these medications in order to tailor them to the patient.12
Educational financial support for this Satellite symposium was provided by Lundbeck.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.