Two functional magnetic resonance imaging studies to find out what happens to the brain in patients with migraine during the different phases of a migraine attack and over 4 years were presented at EAN 2020. One suggested that there is a complex interplay of brain networks during a migraine attack, and the other suggested that the brain adapts over time to reduce the frequency of migraine attacks.
Hypothalamic activity and its connectivity with the brainstem play a role in migraine pathophysiology,1 but little is known about how this activity changes with each phase of a migraine attack and over time in people who have migraines.
What happens in the brain during a migraine from prodrome to post-drome?
Migraine episodes appear to result from a complex cyclic interplay of brain networks
To investigate brain activity during a migraine attack, Daniel Martinelli of the University of Pavia, Italy, carried out a pilot study using advanced fMRI. He evaluated resting state functional connectivity (RSFC) in the brain in each phase of a nitroglycerin-induced migraine attack in patients with episodic migraine.
Four RS fMRIs were obtained — at baseline, during the prodrome, during the migraine itself and during the postdrome in five patients with episodic migraine and in four healthy subjects.
A seed-based component analysis was then carried out to rank the strongest coupling of brain regions during the attack.
The main findings of the study were:
- altered functional coupling between brain stem elements involved in pain and the thalamus and hypothalamus, particularly during the prodromal phase
- altered coupling between the thalamus and the frontal, temporal and cerebellar cortex, during the migraine phase
Dr Martinelli therefore suggested that a migraine attack does not appear to result from a single brain stem generator but from a complex cyclic interplay of brain networks.
What happens to the brain of patients with migraine over 4 years?
The brain appears to adapt to reduce the frequency of migraine attacks
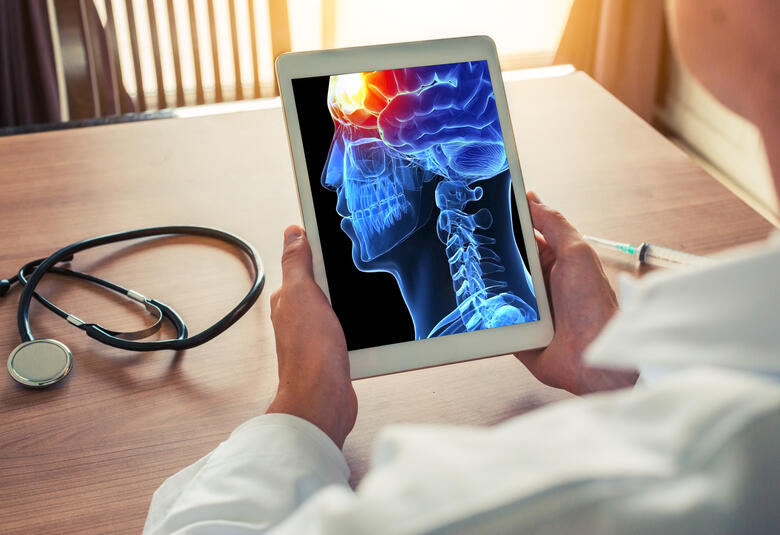
To find out what happens to the brain of patients with migraine over 4 years, Roberta Messina, Vita-Salute San Raffaele University, Milan, Italy and her colleagues mapped cross-sectional and longitudinal hypothalamic RSFC changes using seed-based correlation analysis in 91 patients with migraine and 73 controls over 4 years.
At baseline, patients with migraine had lower hypothalamic RSFC than controls.
After 4 years, the RSFC between the hypothalamus and brain areas belonging to the descending pain inhibitory pathway had strengthened among the 23 patients with migraine who completed the study.
Dr Messina suggested that this strengthening of the RSFC might represent an adaptive response to reduce the frequency of migraine attacks.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.