It has been known for some time that factors such as longer duration of untreated illness are grossly associated with worse outcome. However, no marker per se is sufficiently sensitive or specific to predict outcomes following a first psychotic episode and individualization of treatment remains an enigma. Or does it? #SIRS progress seems to be being made although it might also be raising some interesting challenges for the future.
Three basic issues have limited the progress in the identification of neurobiological illness subtypes that underpin the individualization of treatment:
- studies of first episode psychosis (FEP) have usually been undertaken in patients diagnosed with schizophrenia which, despite its exhibiting heterogeneity in its disease course, does not cover all psychoses
- the measures used to assess outcome have been diverse
- the variety of approaches used to identify clinical and neurobiological predictors have not been integrated in a coherent mechanistic framework
In this symposium, means of defining more precise clinical and neurobiological subtypes were presented.
Morphological cluster analysis in patients with schizophrenia
Professor Lena Palaniyappan, Department of Psychiatry and Medical BioPhysics, London, Ontario, Canada, described two studies which suggest that patients with schizophrenia cluster into morphological subgroups with distinct clinical characteristics.
In the first study, cross-sectional diffusion tensor imaging was used (DTI) to compare 70 patients with schizophrenia and 77 controls.1 Patients had a significantly lower topographic diversity than controls, despite being highly dissimilar from each other. This study’s authors suggest that there is a highly individualized pattern of structural disconnectivity that underlies the heterogeneity of schizophrenia, but such disruptions probably converge on a common pathway that promotes the clinical phenotype. As Professor Palaniyappan summarized, every patient with schizophrenia is alike in having a disconnected brain, but for each the connectivity is altered in its own way.
Every patient with schizophrenia is alike in having a disconnected brain, but for each the connectivity is altered in its own way
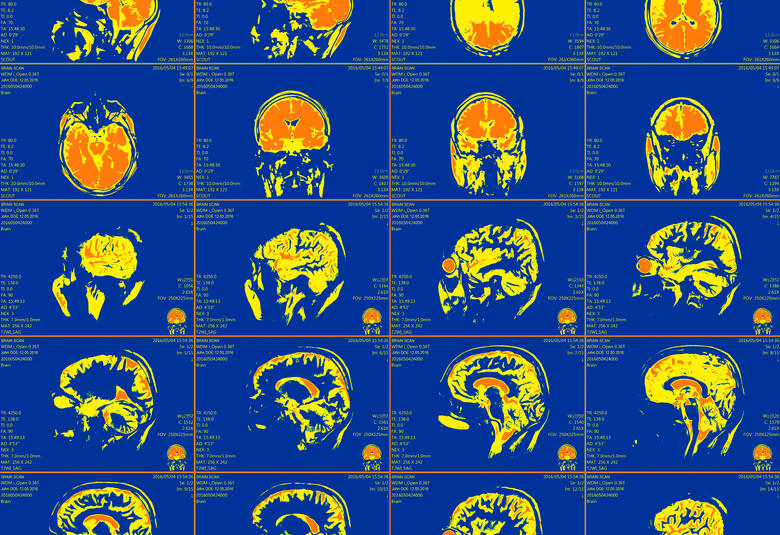
In the second study, structural MRI scans measured cortical thickness in 179 patients with schizophrenia and 77 controls.2 Three clusters with distinct regional thickness patterns were identified: morphologically impoverished (25% patients; 1% controls), intermediate (47% patients; 46% controls), and intact (28% patients; 53% controls). A variety of clinical features was compared in each cluster, including age of onset, total burden of positive symptoms and severity of delusion. Specifically, the impoverished group showed deficits in the N-back test and a less severe positive symptoms burden. It was suggested that such MRI-guided stratification could be used in a biomarker in clinical studies.
MRI-guided stratification of cortical thickness could be used in a biomarker in clinical studies
Genetics and neuroimaging – more powerful together
The research described by Professor Tao Li, Sichuan University, Chengdu, China, adopts a cross-disorder approach, which integrates genetics and neuroimaging.3 She reported that a common pathophysiology existed among three common psychiatric illnesses – schizophrenia, bipolar disorder and depression – with the ZNF391 gene being the potential driving force. New biotypes could be defined based on the spatial expression pattern of this gene.
A gene driven common pathophysiology existed among three common psychiatric illnesses – schizophrenia, bipolar disorder and depression
Lessons from oncological research
Dr Dominic Dwyer, Ludwig Maximillian University, Munich, Germany, has adopted an approach used in oncological studies called “spare non-negative matrix factorization (SCMF)”. Thousands of clinical and other variables can be investigated to identify clusters of patients with tumor subtypes using this technique: it has facilitated personalization of medicine in oncology.
Using SCMF on data gathered from 765 patients with predominantly schizophrenia and bipolar disorder diagnoses, five subgroups were detected with different clinical signatures, illness trajectories and genetic scores for educational attainment. Thus, it may be possible to group patients by prognosis.
PHENOM consortium
Professor Paola Dazzan, King’s Hospital, London, UK, gave a valuable review entitled ‘Dissecting the heterogeneity of psychosis’ and suggested it might be time to let the neurobiology tell us about the outcome rather than vice versa. She cited the work of the PHENOM consortium which used a machine learning approach when lead to the identification of two distinct neuroanatomical subtypes of chronic schizophrenia, only one of which has a progressive course of illness.4
It might be time to let the neurobiology tell us about the outcome rather than vice versa
Moving forward, she suggested that studying the predictors of an illness’s course based on pre-specified cut-off points for remission and relapse can lead to misclassification. As static categories with single trajectories apply only to a minority of patients, the point at which biomarkers are evaluated also needs careful consideration. As marked changes in the course of symptoms can occur even 3-5 years after onset, information on illness course should be acquired over long follow-up periods.
Studying the predictors of an illness’s course based on pre-specified cut-off points for remission and relapse can lead to misclassification
She concluded by suggesting that using traditional categories of illness course will really hinder attainment of knowledge of the neurobiology of psychoses and will limit the identification of the best individualized approach to treatment.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.