Biomarkers are available and used effectively in other disorders– notably some of the cancers – but they remain elusive in schizophrenia. An early morning brainstorming session discussed some of the reasons for this, and some potential candidates.
What are biomarkers, and why do we want them?
Professor Florence Thibaut (University Hospital Cochin Paris, Sorbonne-Paris Cité University, France) first described what we might mean by ‘biomarker’. This can be an indicator of the presence of a disease, or of its pharmacological response to treatment. The first type may be used to identify non-affected people who are at an increased risk of developing the condition, possibly therefore allowing early diagnosis and treatment. Other types of biomarkers may relate to treatment susceptibility, and/or disease severity and trajectory. These can be used to develop individualized treatment strategies. All biomarkers need to be sensitive and selective – to allow an accurate and specific diagnosis – as well as non-invasive, inexpensive and reproducible across centers.
All biomarkers need to be sensitive and selective – to allow an accurate and specific diagnosis
Endophenotypes to identify people with schizophrenia
Endophenotypes in schizophrenia represent a move towards biomarkers. These are quantifiable biological variations or deficits between individuals, which are presumed to reflect an inherited vulnerability to the disorder. Several neurophysiological endophenotypes associated with schizophrenia have been identified. Prof Thibaut discussed measures from smooth pursuit eye movement tests (an anti-saccade paradigm sensitive to dysfunction or damage to the frontal lobe) and event-related potentials that have shown some sensitivity for schizophrenia. These measures are also stable over time (and therefore likely to reflect disease traits rather than states). Prof Thibaut noted that changes on these parameters are also seen in other psychiatric disorders, but combining a number of measures may help differentiating patients with schizophrenia from controls in the general population and even from other family members.
Cognitive endophenotypes have also been identified that reflect the cognitive deficits seen in schizophrenia. Changes on the California Verbal Learning Test,1 and the Wisconsin Card Sorting test2 have both been reported in patients with early schizophrenia. The state-independence, stability over time and magnitude of deficit in these two measures makes both them potential candidates for use in schizophrenia.
Neurophysiological and cognitive endophenotypes have been identified in schizophrenia
Genetics may hold some keys to unlock the disease process
Professor Dr Dan Rujescu (Martin-Luther-Universität Halle-Wittenberg, Germany) explained that he was focusing on genetic candidates as biomarkers for schizophrenia. He said that on the one hand researchers in this area are fortunate, because schizophrenia is a syndrome that has such a large genetic component (70–85% heritability). However, on the other hand, schizophrenia and other psychiatric disorders are much more heterogeneous in terms of their genetics than, for instance, common neurological disorders. There is also a large overlap in genetic markers between schizophrenia and other psychiatric disorders, which makes it difficult to identify specific disease markers. Nevertheless, markers those that have been identified may help us understand the pathophysiology of this complex disorder, and point to new treatment strategies.
Schizophrenia shows a high degree of heritability, but also large genetic heterogeneity
Genetic candidates for biomarkers
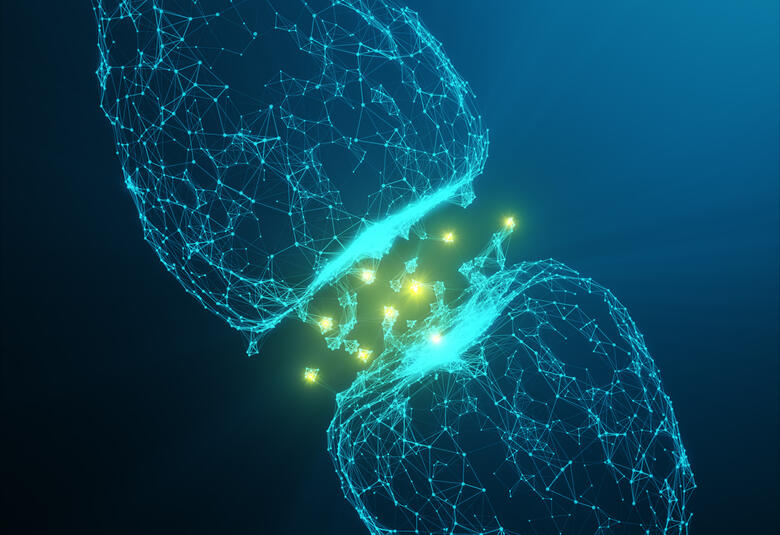
Prof Rujescu gave an example of a deletion in the gene encoding Neurexin 1 that has been identified in schizophrenia. Neurexins are presynaptic adhesion molecules that are involved in the stabilization and plasticity of glutamatergic and GABAergic neurons. These, and other results, point towards the fact that the dopaminergic hypothesis of schizophrenia describes only part of the whole story, and the pathophysiology of this disorder clearly also involves glutamate and GABA.
There is a large overlap in genetic markers between schizophrenia and other psychiatric disorders, which makes it difficult to identify specific disease markers
Some of the genetic changes identified so far in schizophrenia are found in only a small number of patients. They would not, therefore, be appropriate for population screening, but might make such patients candidates for personalized treatment strategies related to their phenotype. When more common and specific genetic biomarkers have been identified, it may be possible to stratify patient populations for different treatment approaches.
Some of the genetic changes identified so far in schizophrenia are found in only a small number of patients
In conclusion, biomarkers in psychiatric disorders remain an active area for research. Some promising candidates have been identified, leaving one optimistic about the promise of early disease identification and individualized treatment in the future.