Consortia the world over are seeking biomarkers, including abnormalities on brain imaging, that reliably predict transition to psychosis in at-risk individuals and response to treatment in those with schizophrenia. They are also on the look-out for markers that may relate disease categories more reliably to underlying biology. What have they been finding?
In psychosis (as in other areas of mental health), our traditional diagnostic categories seem not to correspond to underlying neurobiology. The belief that this might be the case led to the promotion of an alternative system of classification -- the Research Domain (RDoC) Criteria -- which considers problems as lying along trans-diagnostic domains such as social and cognitive functioning, arousal, negative valence (threat, anxiety, loss) and positive valence (motivation and responsiveness to reward).1
Support for this broad perspective now comes from the Bipolar-Schizophrenia Network for Intermediate Phenotypes (B-SNIP) study,2 as described at ECNP by Godfrey Pearlson (University of Yale, New Haven, Connecticut, USA).
Applying machine learning techniques to basic clinical and biological data classifies psychoses better than DSM
Three stable biotypes
Building a model from the bottom up, by applying machine learning techniques to clinical and biological data, can improve the classification of psychoses, he told at the meeting.
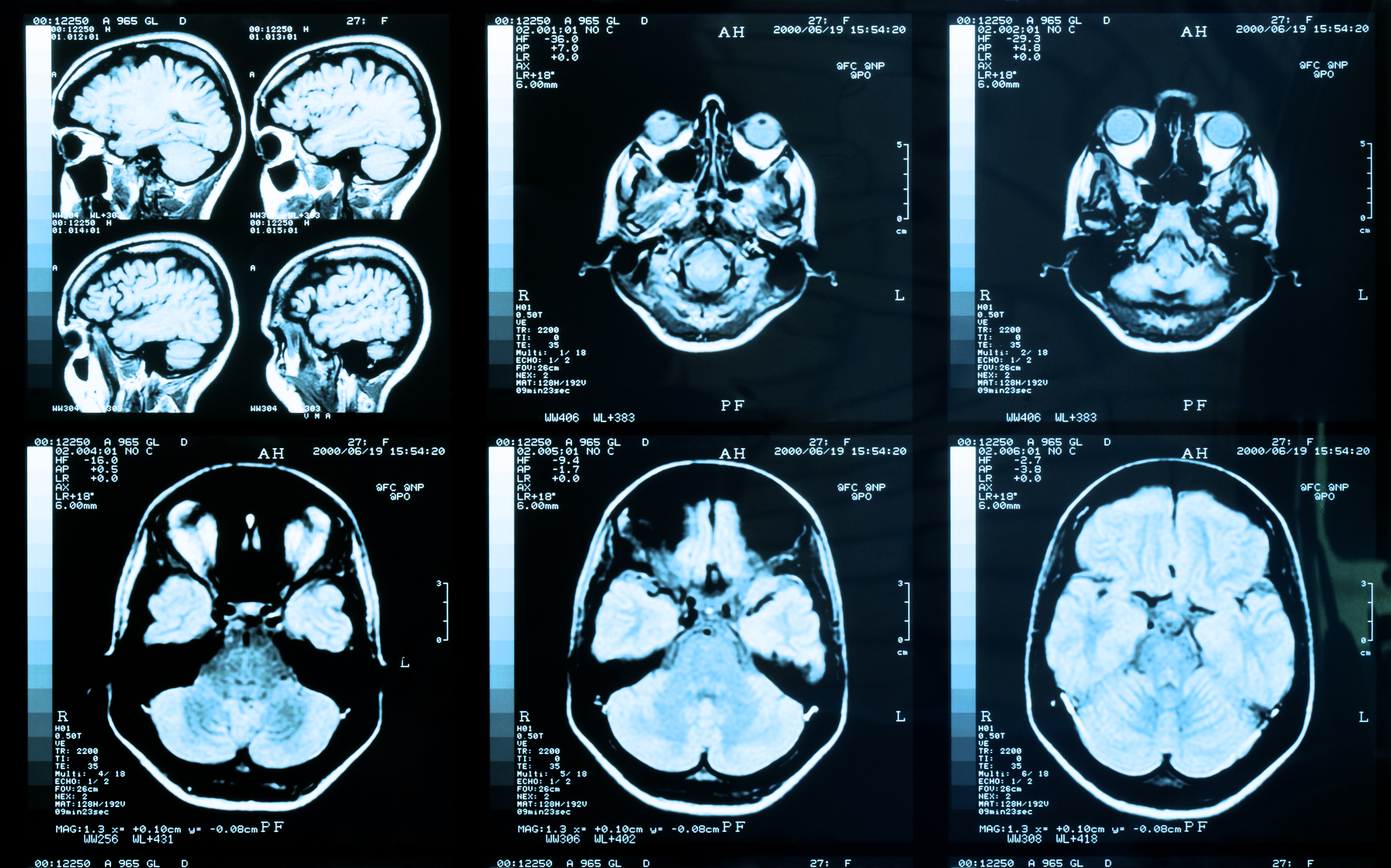
B-SNIP’s starting point was to take approaching 1000 patients with 1 of 3 conventional diagnoses – schizophrenia, schizoaffective disorder and psychotic bipolar disorder – and measure a wide range of cognitive variables, electrophysiological variables such as auditory evoked potentials, and aspects of eye movement, along with structural and functional MRI.
Bottom-up analysis suggested that patients could reliably be divided into one of three robust biotypes that were largely independent of traditional clinical diagnostic classifications.
Biotype 1 patients were the most cognitively impaired and also differed from healthy controls in social functioning and brain volume. Biotype 2 patients had sensorimotor reactivity and intermediate levels of impaired cognition. Biotype 3 patients resembled most closely healthy controls, were the least socially impaired, and had the lowest levels of positive and negative symptoms. Interestingly, they tended to have a history of cannabis use, Professor Pearlson told attendees at ECNP.
The next step is to see if the different biotypes respond differently to treatment
Mixed results in success of imaging
It’s difficult to make predictions, especially about the future. The origins of the saying are contested. Its truth is not – as was freely admitted by Andrew Lawrence (King’s College, University of London, UK) when presenting imaging findings from the OPTiMiSE project in first-episode schizophrenia.
Though essentially a treatment study, OPTiMiSE, which included 481 patients aged 18-40 with untreated symptoms for less than two years and less than two weeks’ lifetime exposure to antipsychotics,3 had a functional MRI component.
Baseline structural MRI variables did not predict outcome at four weeks in treated first-episode psychosis
The 201 patients studied had a baseline, pre-treatment MRI. This was assessed in relation to outcome at four weeks, using PANSS criteria, at which point 68% of patients in this subset were considered to be in remission. Various structural brain measures were used, notably mean cortical thickness in 31 regions, surface area and a local gyrification index of cortical folding. There were also measures relating to subcortical regions. The bottom line is that none of these baseline MRI measures predicted clinical outcome.
Structure and connectivity
Study of high clinical risk group shows abnormal connectivity pattern predicts conversion
Perhaps, Dr Lawrence speculated, four weeks is too short to assess any correlation. Perhaps the study was compromised by heterogeneity in imaging and assessment between the many sites involved. Or perhaps brain structure is simply not that a good predictor, and other imaging modalities – or different biomarkers entirely, such as those relating to inflammation -- would give us a better handle on processes underlying the disease and its response.
A second context in which prediction would be highly useful is in distinguishing people at high risk of having a first episode of psychosis. And it seems that increased connectivity in a cerebellar-thalamo-cortical network is indeed predictive of conversion to psychosis in people at clinically high risk, according to data from the NAPLS study presented by Tyrone Cannon (University of Yale, New Haven, Connecticut, USA).
Abnormality of brain architecture – which can be seen in both task-related and resting states -- is more pronounced among converters than non-converters and predicts time to conversion
Investigators from the North American Prodrome Longitudinal Study consortium have demonstrated that this abnormality of brain architecture – which can be seen in both task-related and resting states -- is more pronounced among converters than non-converters and predicts time to conversion. By way of validation, they have also confirmed that this pattern of hyperconnectivity is present in patients with established schizophrenia.4