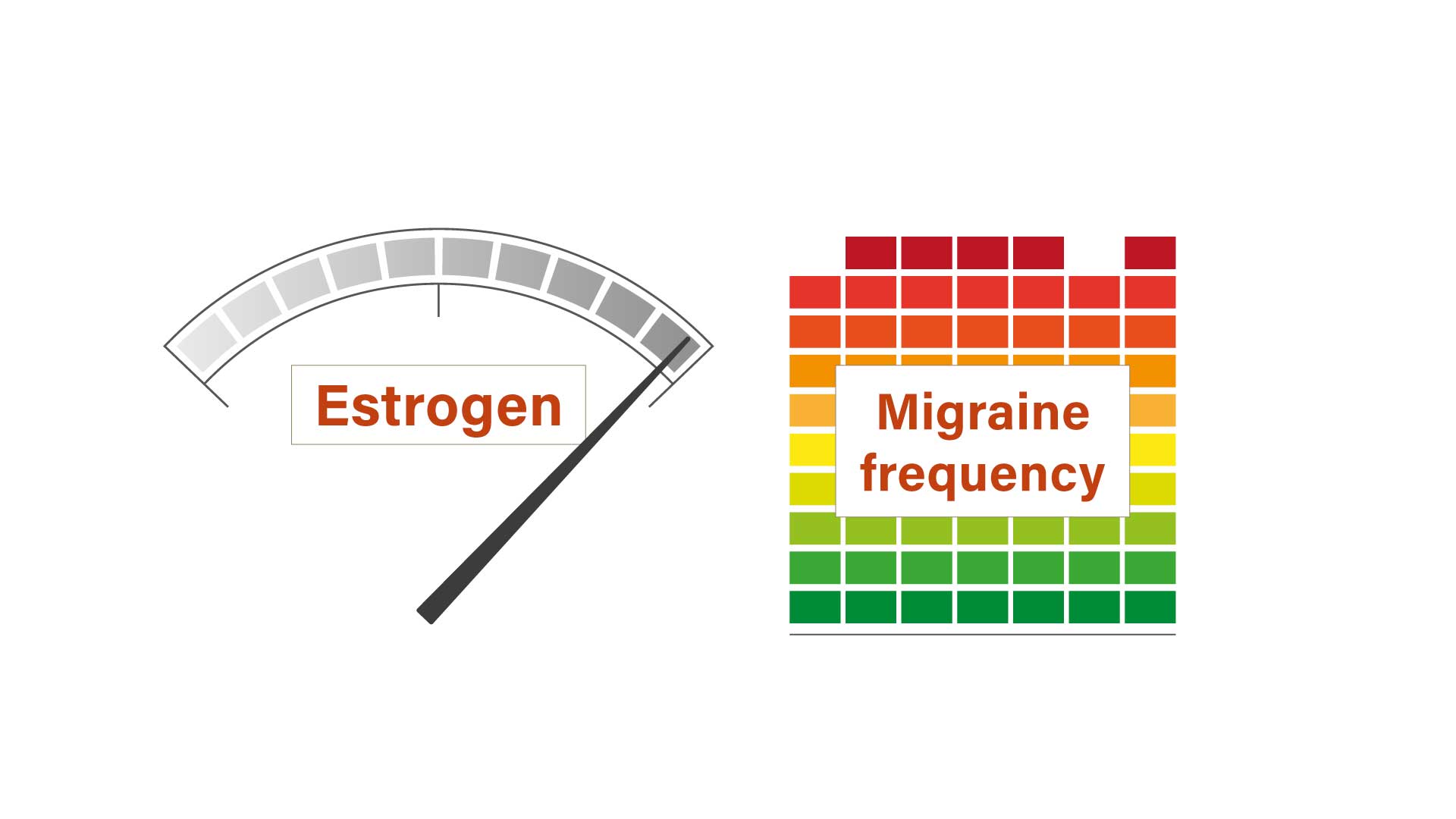
Migraine is twice as prevalent in women than in men.1 Estrogen is a predisposing factor with decreasing levels associated with increased frequency of migraine episodes. The associations between estrogen and migraine and why changing estrogen levels are linked to migraine episodes were explored by Patricia Pozo-Rosich, University of Barcelona, Spain, in an online presentation for live EAN 2020.
Why is migraine more common in women?
Menstruation is a risk factor for migraine without aura
Among 40,000 people who participated in the 2003 National Health Interview Survey in the US the prevalence of migraine was 9% in males and 18% in females,1 said Dr Pozo-Rosich. It is highest in women between puberty and the menopause,2 reaching a peak of 25% among women in their thirties and forties.3
Changing estrogen levels are linked to migraine epsiodes
Changing estrogen levels associated with menarche, oral contraceptive (OC) use, pregnancy, lactation, and menopause are frequently accompanied by changes in the patterns and frequency of migraine:4
- decreasing estrogen levels at the onset of menses, during the pill-free interval with OC use, and postpartum are associated with increased frequency of migraine episodes
- increasing or stable estrogen levels during pregnancy, while taking OC, and after the menopause are associated with decreased frequency of migraine episodes4
Perimenstrual migraine episodes are less responsive to treatment than non-menstrual episodes
Furthermore, menstruation is a risk factor for migraine without aura attacks, said Dr Pozo-Rosich, and can be the only or primary trigger in up to 14% of patients.5
Perimenstrual migraine episodes are longer and less responsive to treatment than non-menstrual episodes.6
Why can estrogens cause migraine?
Estrogens cause changes in the circulation, nociception, and the brain
Estrogens appear to cause migraine through a variety of mechanisms including:
- vasodilatation due to increased endothelial nitric oxide synthase7
- genetic modulation of serotonin levels involved in nociception8
- endometrial synthesis of prostaglandin, which sensitizes nociceptors and promotes inflammation9
- cortical excitability10
ICHD-3 criteria for diagnosing migraine related to menstruation
For better characterization of migraine associated with menstruation the Appendix of International Classification of Headache Disorders 3rd edition (ICHD-3) offers criteria for diagnosing pure menstrual migraine without aura and with aura, menstrually-related migraine without aura and with aura, and non-menstrual migraine without aura and with aura.11
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.