In November 2014, Cyril Höschl gave a presentation at the Lundbeck Institute on ‘Psychiatry and Culture - Understanding mutual relationships’. Professor Höschl, director of the National Institute of Mental Health in Klecany, Czech Republic, highlighted the influence of culture and society on psychiatry.
Psychiatry has long struggled to find a biological base on which to generate explanatory models of psychiatric disease, including schizophrenia, that are applicable across cultures. The discovery of effective psychopharmaceuticals and advances in functional neuroimaging show that aspects of psychiatry do have a clear biological basis. But, psychiatry, and indeed medicine in general, can only be fully understood when considered within the context of the culture in which it is practised.
Human beings and their reality are socially constructed
Socio-cultural factors relate to psychiatry by:
-
influencing the pathogenesis and symptomatology of psychiatric illness
-
influencing our response to it
-
underpinning and legitimising psychiatric and other interventions.
Cross cultural differences
Psychiatry is a culture-specific system of knowledge, power and institutions. Those with an interest in mental health wish to accumulate knowledge of how to make an accurate diagnosis and manage patients. However, the culture in which psychiatry is practised helps determine what constitutes a psychological condition and influences symptomatology.
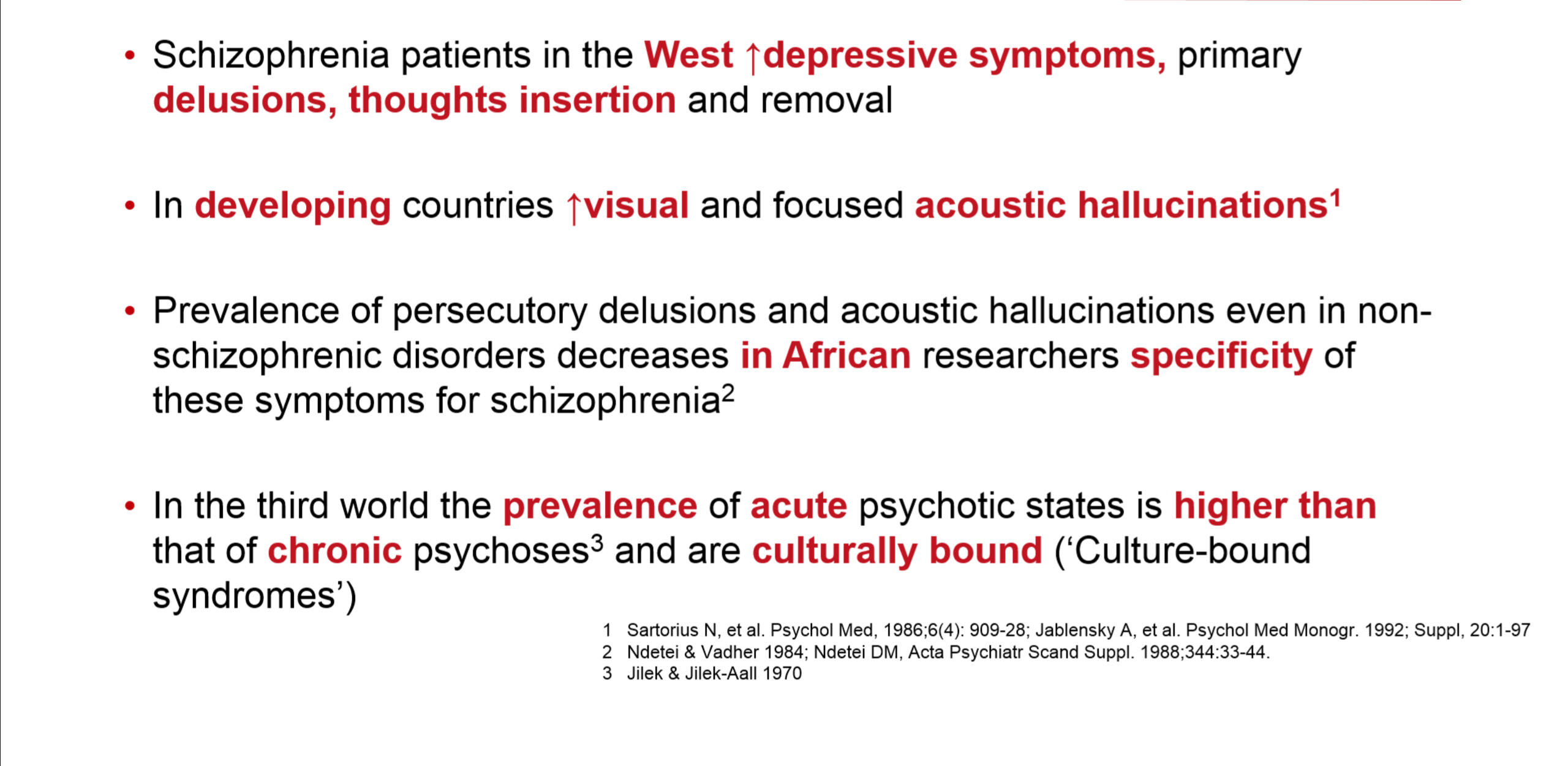
There are differences between cultures in the prevalence of persecutory delusions, even in non-schizophrenic disorders, and of acute psychosis, much of which is culturally bound. For example, in Western Africa and Latin America, paranoid delusions and hallucinations are often triggered by an intense fear of magical persecution and witchcraft. In Indonesia and Malaysia, the stressor is fear of loss of fertility through ascendance of the penis into the abdomen.
These conditions are real within the cultures in which they occur – pain and physical symptoms are experienced – even though no physiological basis for them has yet been described.
In the West, patients with schizophrenia exhibit a greater level of depressive symptoms, primary delusions and thought insertions and removals than patients in developing countries. Conversely, patients in developing countries experience more visual and acoustic hallucinations than their Western peers.1,2
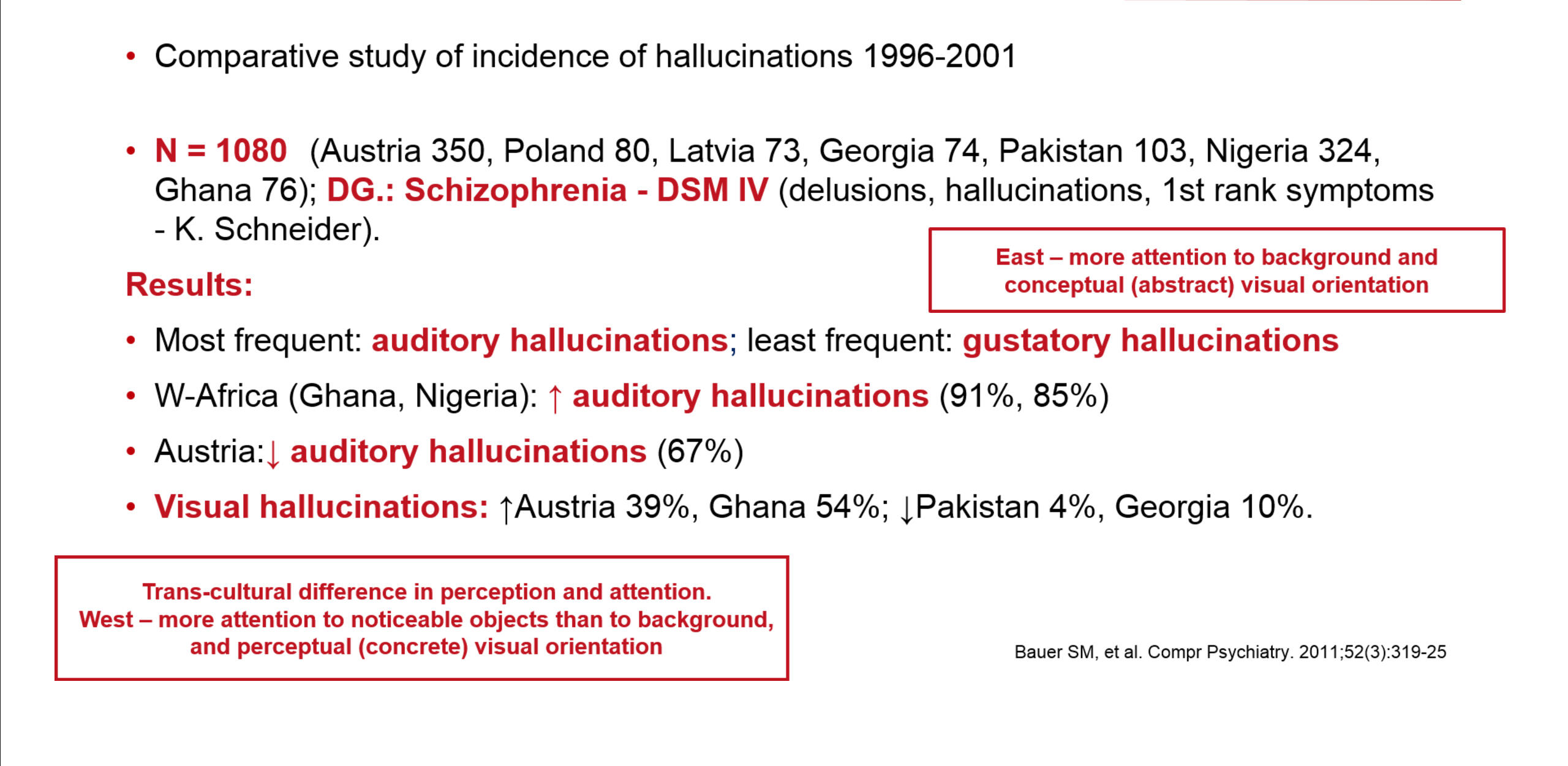
In a recent study a total of 1080 patients from Austria, Poland, Lithuania, Georgia, Pakistan, Nigeria and Ghana were diagnosed with schizophrenia using DSM-IV criteria.3 Not only were differences in the incidence of each type of hallucination reported (auditory hallucinations were most common; gustatory hallucinations the least), but pronounced differences in patterns between the countries were also observed.
The study’s authors concluded that the difference in the visual hallucination rate noted between Westerners and East Asians was likely due to cultural differences in perceptual and attentional processing. They noted that Westerners pay more attention to salient objects in an image than its background, unlike East Asians who pay more attention to the image’s background. They reasoned that this difference in visual processing could account for the difference in hallucination type between these groups.
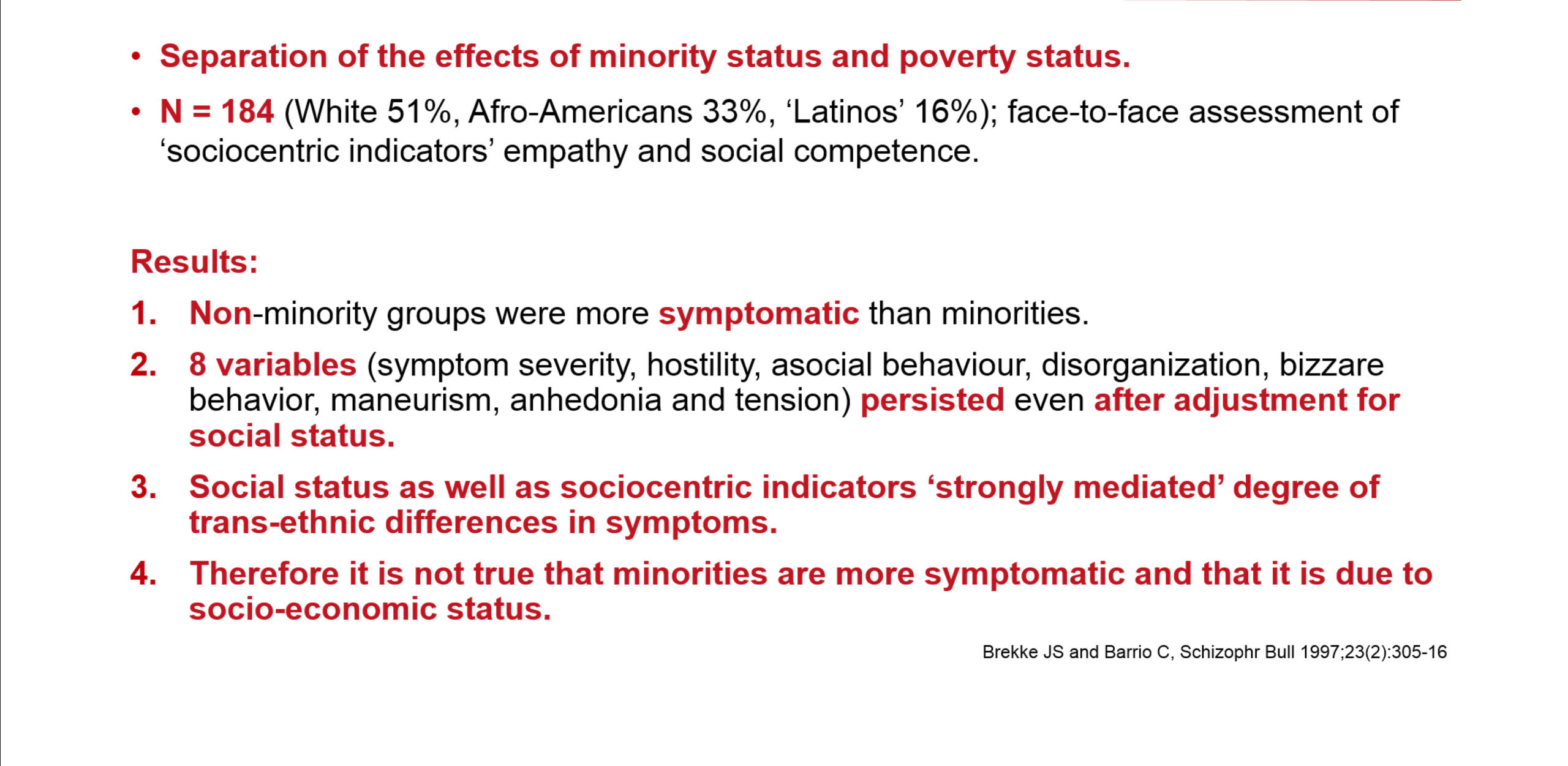
Sociocentricity (defined as orientation toward society; based on social factors) is an important concept in understanding cultural variance in schizophrenia. Brekke and Barrio undertook a study investigating schizophrenia and socioeconomic and minority status in the USA.4 Three groups were compared: Caucasian Americans, Black Americans and Latinos. Surprisingly, the non-minority group was shown to be more symptomatic than the minority groups. The sociocentricity of the minority groups was held to be the ‘protective’ factor responsible for the lower rate of symptoms.
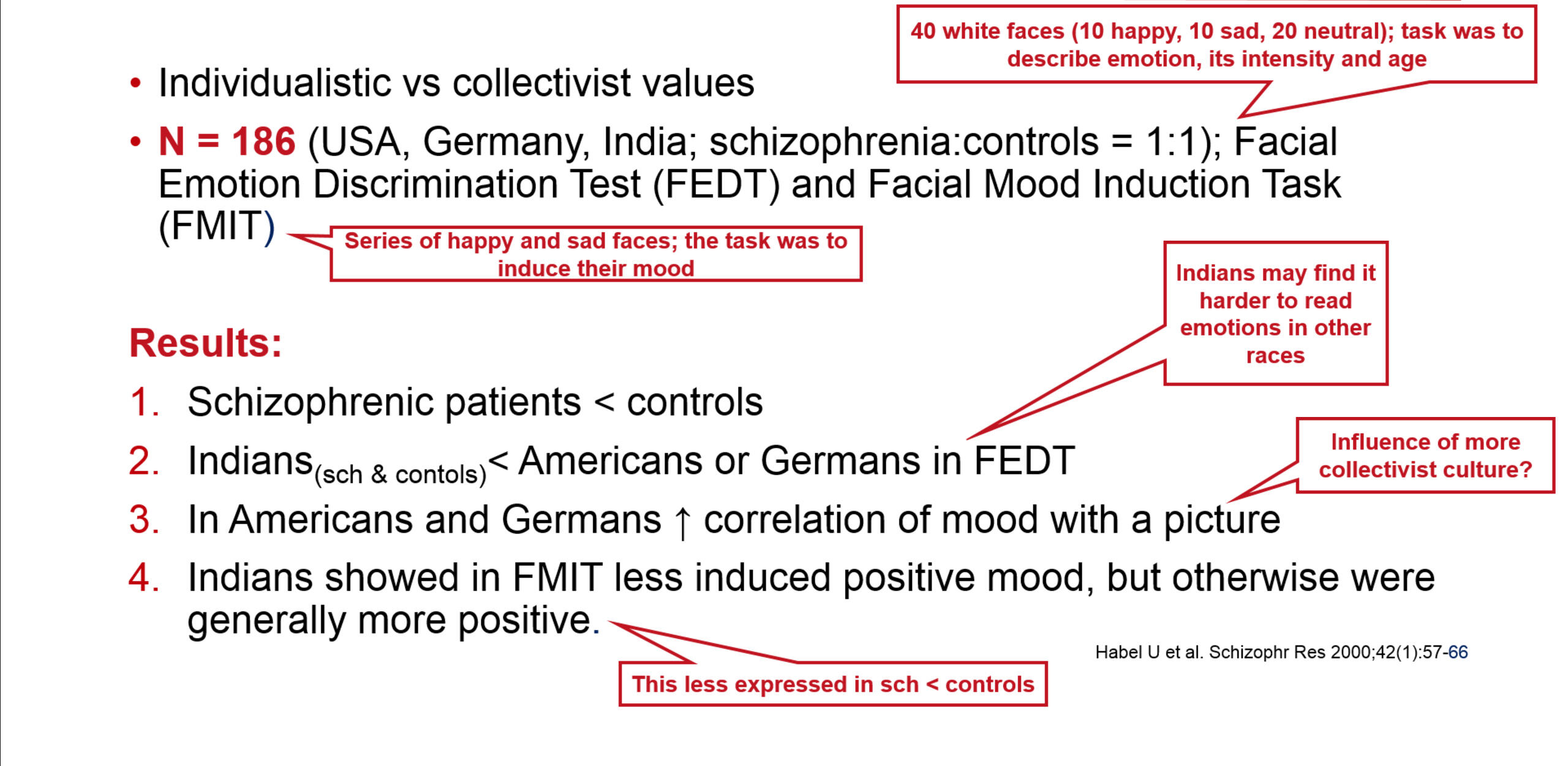
Sociocentricity can also influence the nature of the symptoms exhibited by patients. Habel et al showed that the values of the society can affect emotional processing and mood in schizophrenia.5
Patients and healthy controls from three populations – American, German and Indian – underwent two tests. In the first – the Facial Emotion Discrimination Test – happy, sad and neutral Caucasian faces were shown to study subjects who were asked to identify the emotion displayed. As expected, patients did worse than controls. However, the Indian subjects also seemed less able to judge the emotions of a different ethnic group.
In the second test – the Facial Mood Induction Test – happy or sad Caucasian faces were shown to study subjects who were then asked to emotionally empathise with the image. Here, the Indian groups (patient and control) again behaved differently to the others. Of particular interest was the behaviour of the Indian control group, which responded less negatively to sad images but significantly more positively to happy images than the other groups. Unlike the individualistic nature of American and German cultures, the collective nature of Indian culture, which suppresses negative emotional experiences, is thought to be responsible for this observation.
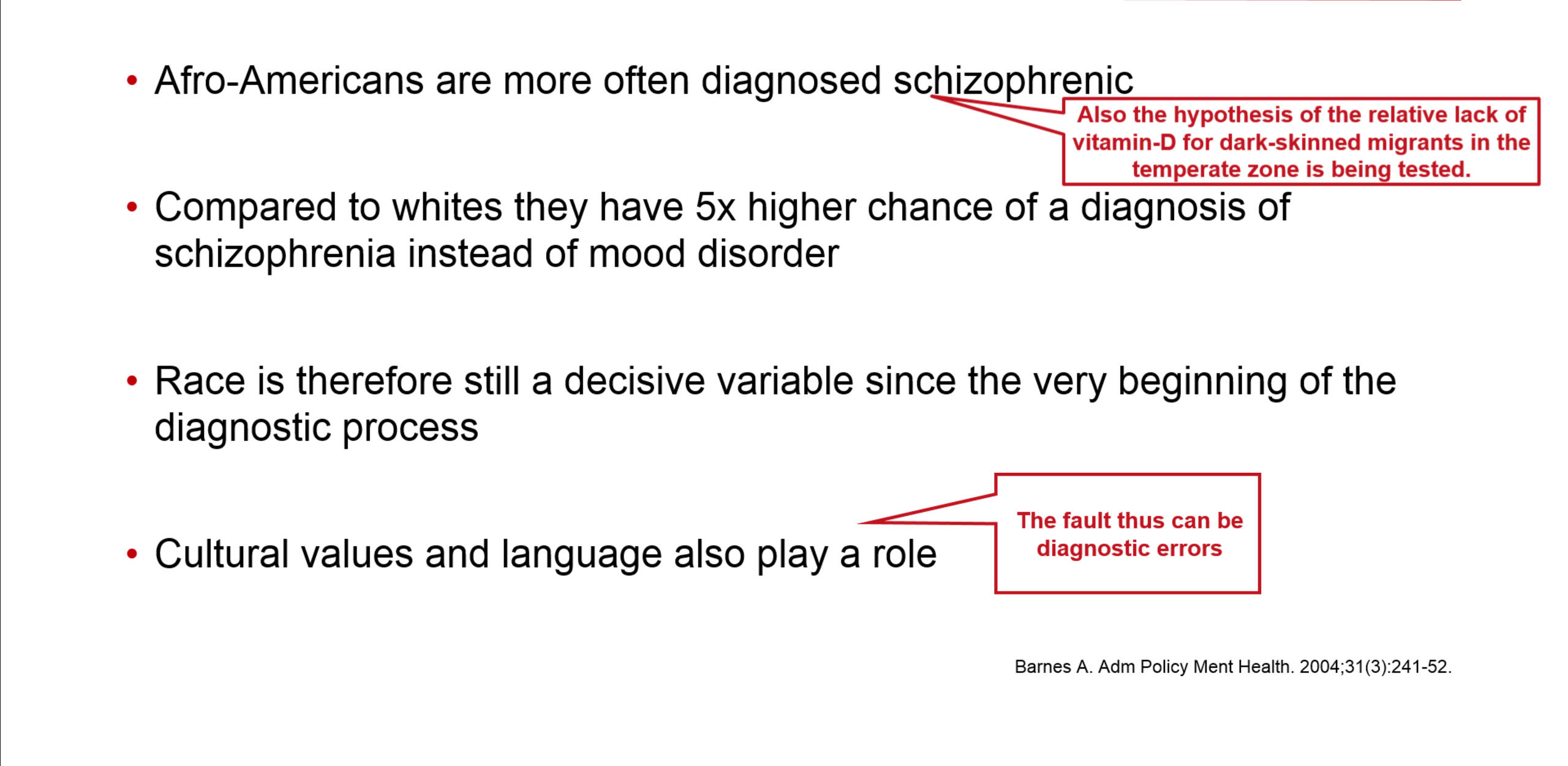
Cross-cultural and racial differences don’t relate solely to symptoms but influence the whole diagnostic process. In the USA, African Americans are five time more likely to be diagnosed with schizophrenia rather than a less severe mood disorder than Caucasian Americans.6
The language psychiatrists use can also hinder or help accurate diagnosis. In Japan, changing the term for schizophrenia from ‘mind split disorder’ to ‘integration disorder’ aided diagnosis considerably. This was because physicians were no longer using euphemisms to describe the disease and because the new terminology was more socially acceptable.
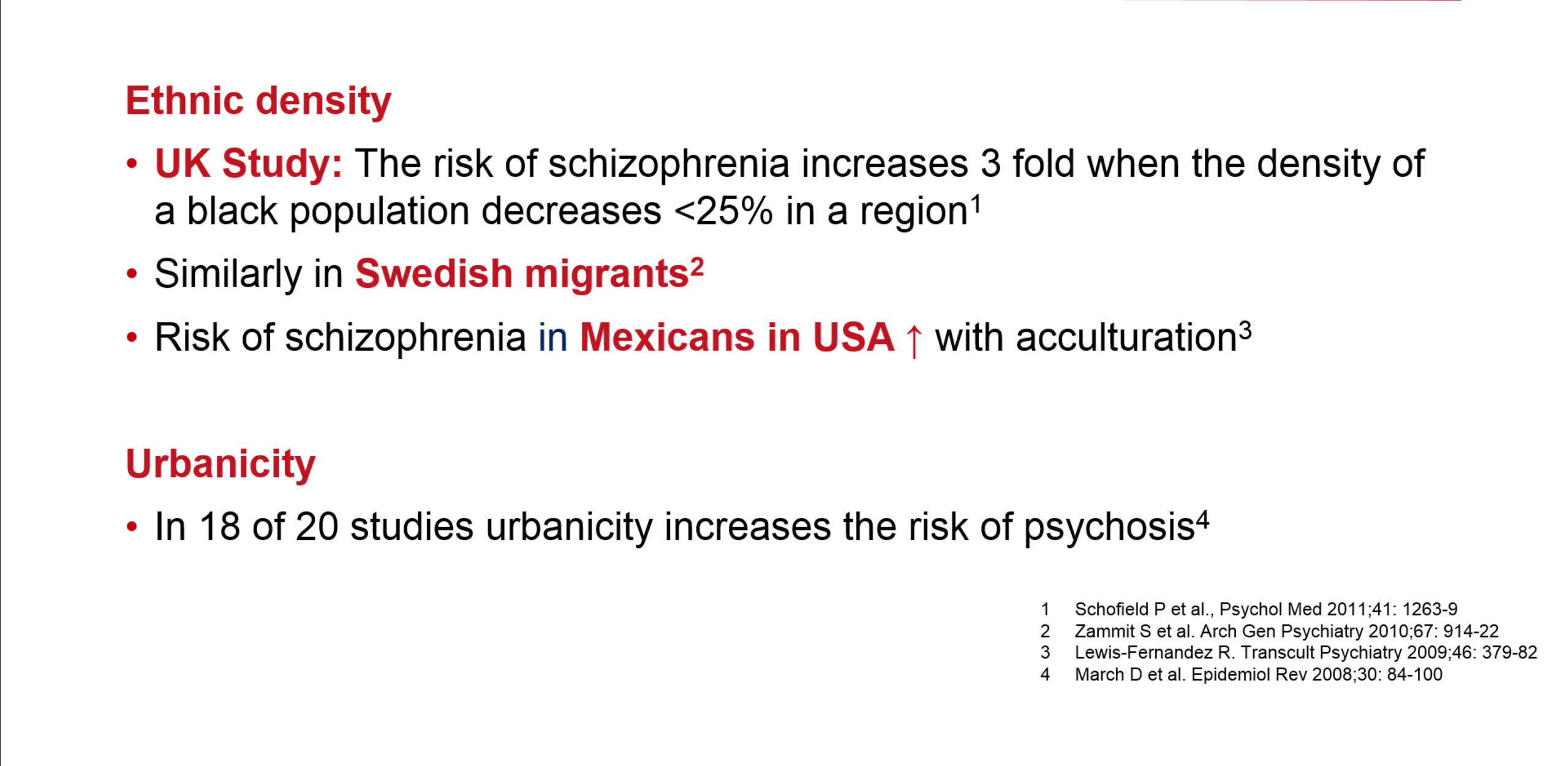
Risk factors for schizophrenia, including ethnic density and urbanicity, also vary with culture. A British study showed that the risk of schizophrenia increases as ethnic density diminishes.7 Similar findings were reported from Sweden and Mexico.8,9 Similarly, urbanicity increases the risk of psychosis.10 The case is not so clear-cut for socioeconomic status as a risk factor since published reports are conflicting.11,12,13.
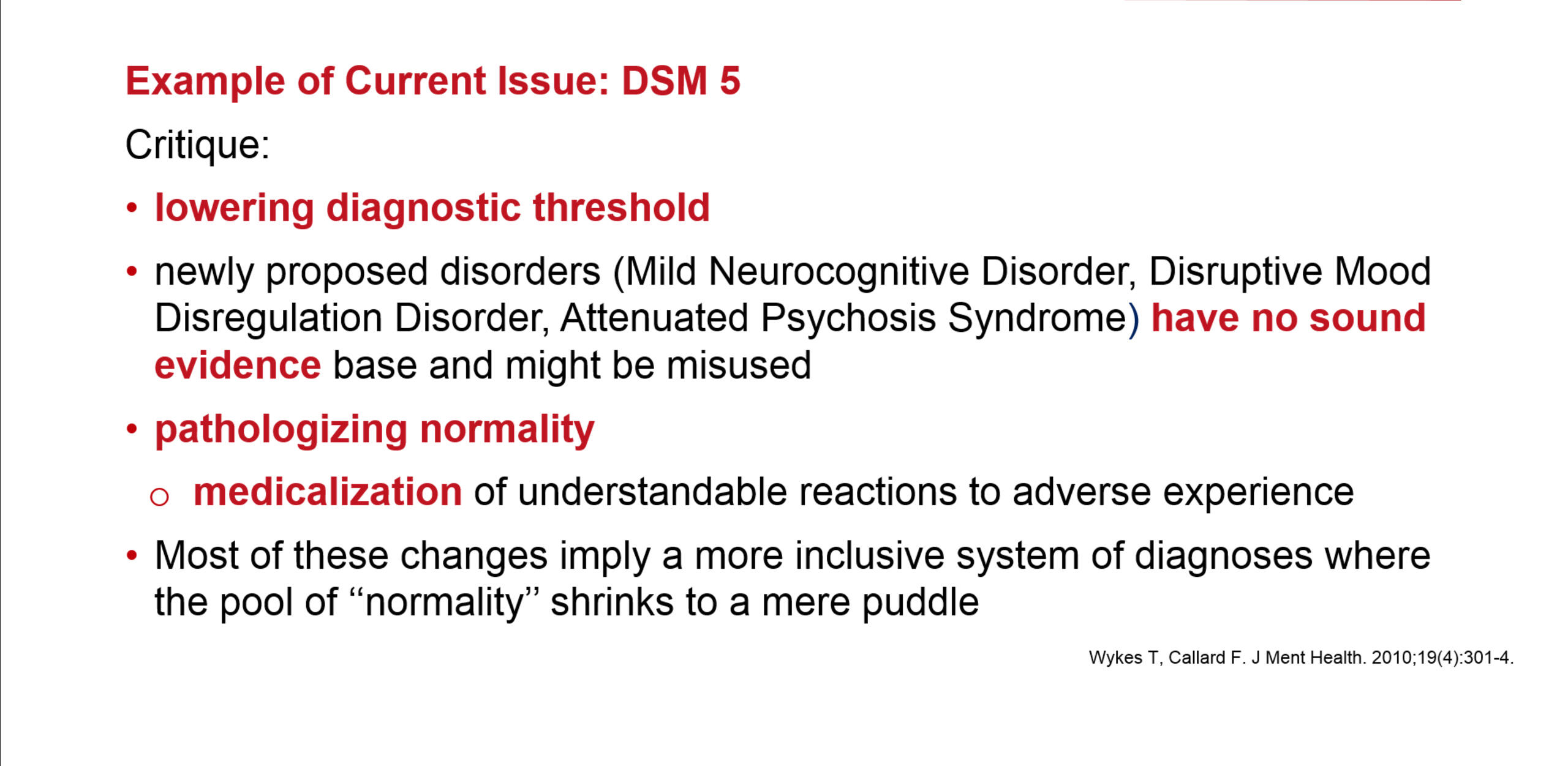
If schizophrenia manifests itself in different ways throughout the world, using tools such as DSM-IV and DSM-5 as the sole means of assessment raises many issues. Ignoring cultural and social differences risks pathologizing normality and may lead to the medicalization of reactions to adverse experiences that – in their context – are understandable.14
Key standard influencers of psychiatry practice throughout the world
Cultural influences on the way mental disorders are perceived, experienced and explained, as well as the institutional context within which they are treated, represent another area of interest to social scientists. The mental health of vulnerable populations is a particular focus.
A meta-analysis of 21 reports investigated the distribution of schizophrenia between the general population and first- and second-generation migrants.15 The increased risk of schizophrenia and related disorders among immigrants clearly persisted into the second generation, suggesting that post-migration factors play a more important role than pre-migration factors or migration per se. The observed variability suggests that the risk is mediated by social context.
Similar conclusions have been drawn by others.16,17 However, the difference in schizophrenia prevalence between the general population and migrant or ethnic minority groups might also be the result of bias arising from the use of diagnostic procedures that are not culturally sensitive.
There may also be confounding environmental factors.18,19 The predominance of schizophrenia among lower social class is now considered to be a consequence of the illness (through unemployment and downward social drift) and not a factor contributing towards it.
It is clear that while schizophrenia is found throughout the world, and while some symptoms are identical (e.g. negative symptoms, thought disorders and cognitive impairment), there are marked cross-cultural differences in the content of psychotic symptoms, in outcomes and in the frequency of acute episodes.
Reactions to mental disorders
Socio-cultural reactions to mental disorders, which are generally spontaneous or unplanned, can have profound consequences for sufferers. Labelling, stigma, discrimination and the adoption of the sick role may negatively affect the patient’s life.20
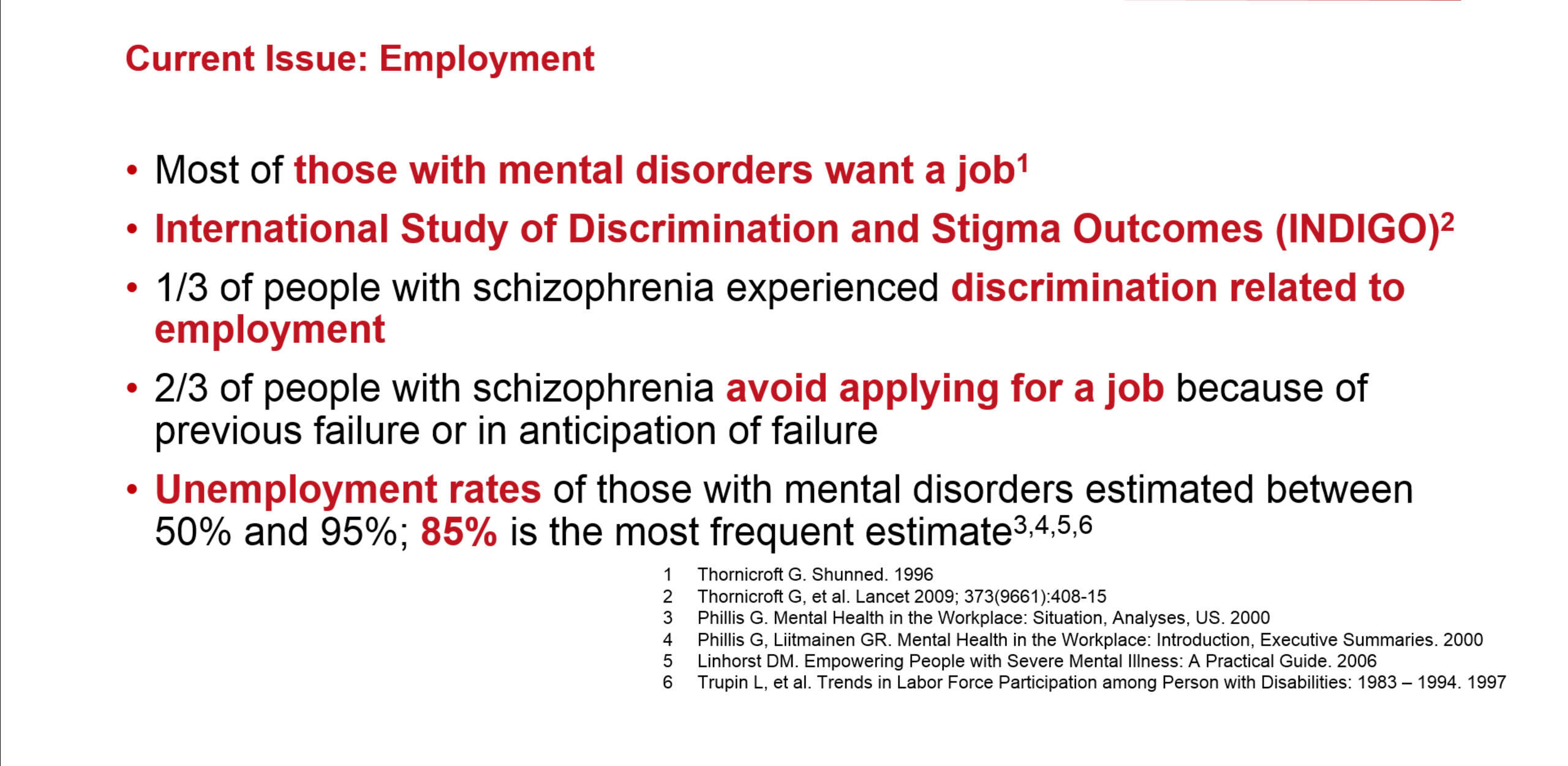
While the majority of those with mental disorders want to work, their employment rate is usually very low.21,22,23,24 Despite European Union and International Labour Organisation policies to reduce unemployment, social stigmatisation and discrimination remain difficult to overcome.
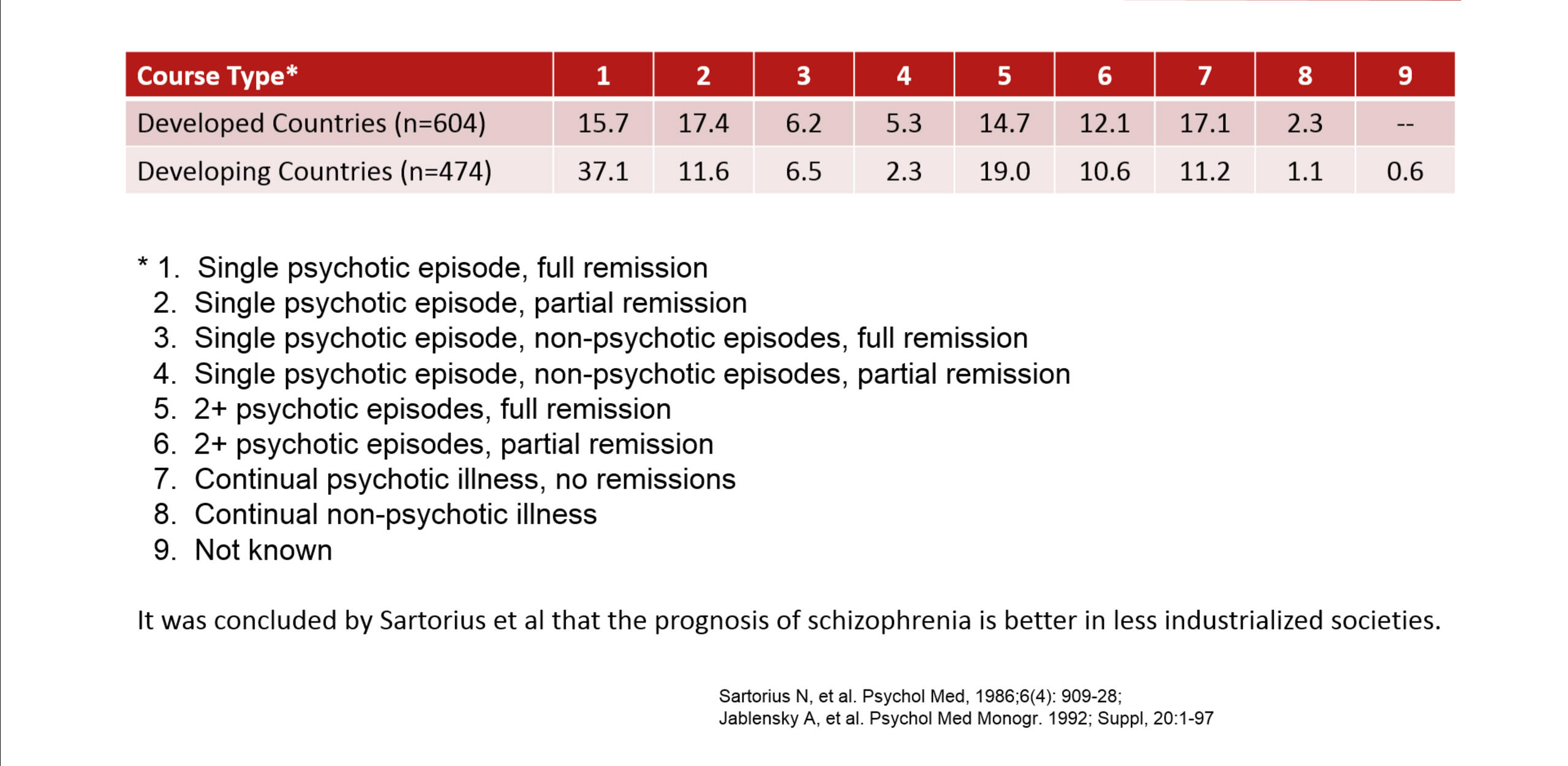
Socio-cultural reactions can differentially impact prognosis. A WHO collaborative study showed that while newly-diagnosed patients from different cultural backgrounds were similar in their symptom profile, the course of the disease over two years was more favourable in those from developing rather than developed countries.1 The reasons suggested are that family and social support are greater; and stress, stigma and pressure to achieve are less in the developing than in the developed world.
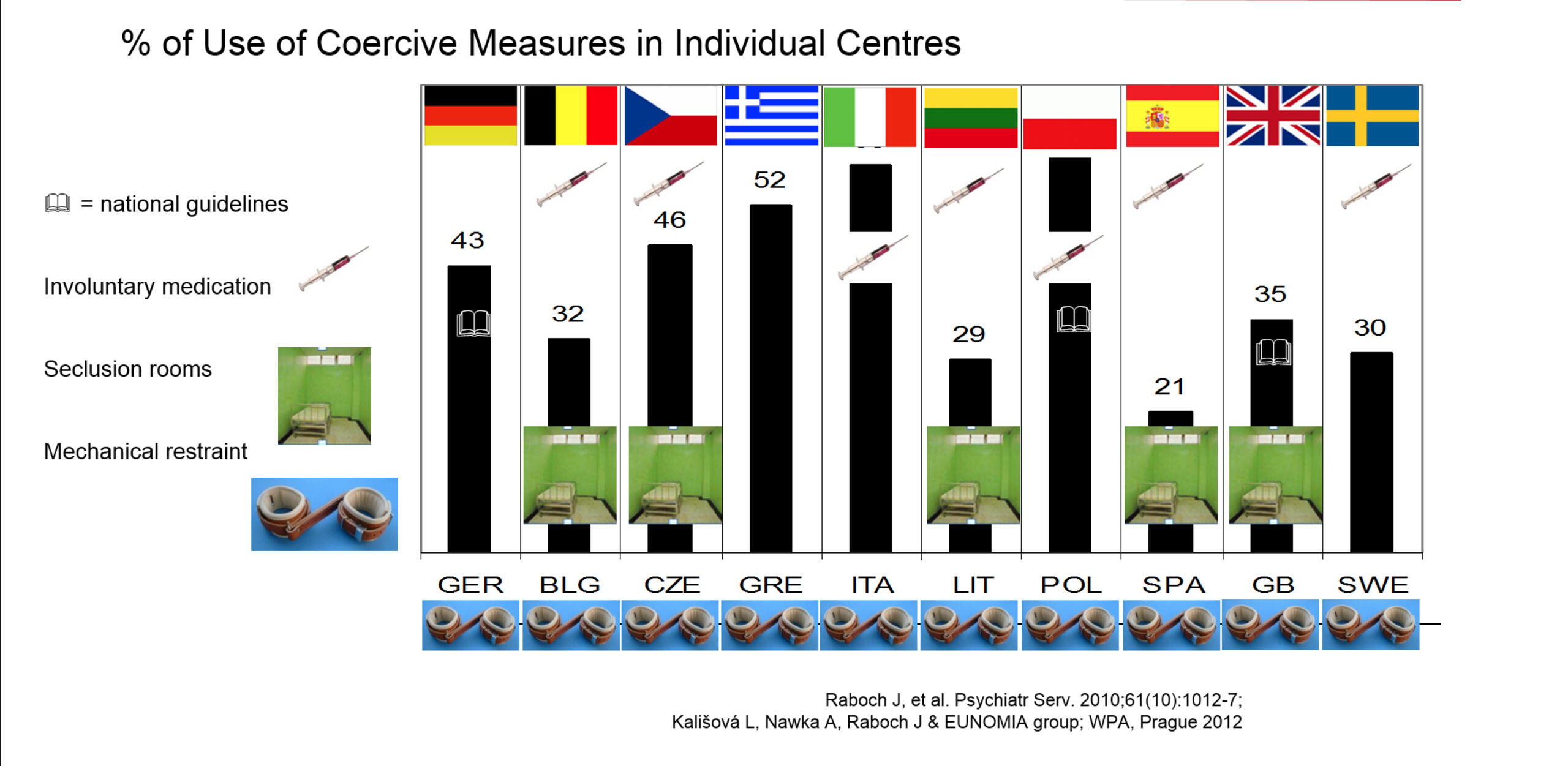
The EUNOMIA project studied the use of coercive measures in involuntarily admitted patients in twelve countries. Overall, 1284 patients with psychotic illness were included, 41% of whom experienced some coercive measure, presumably to mitigate acute psychotic agitation and/or self-harm and aggression.
All the countries studied used coercive measures, but these differed in nature. Involuntary medication was the most frequent (used in seven countries) but was not found in the UK, Germany and Greece. Seclusion rooms were available in only five countries and were most commonly used in the UK. Some kind of mechanical restraint was used in all centres. But, even across Europe, there is cultural variation in the coercive means used to manage patients.25,26
Psychiatry and people with mental health problems do not exist in isolation but within a larger socio-cultural context that influences their nature. This context needs to be taken into account both when treating people with mental health problems and when developing healthcare systems.